Gluten and Neuroinflammation: A New Connection
In recent years, gluten has emerged as a significant dietary concern for a growing number of individuals worldwide. This trend is fuelled by an increasing body of research that highlights the relationship between gluten consumption and a range of health issues, including brain inflammation, obesity, and poor gut health.
The Central Nervous System - The Brain
The brain is a marvel of biological engineering, made up of an intricate network of billions of neurones that enable the complex functions we associate with thought, emotion, and behaviour. Like a computer, it can conduct millions of processes a second, many of which we are not even aware of.
The role the brain plays in our overall health and well-being is so important that when things go awry, we first experience cognitive dysfunction and a sense of malaise.
The brain is shielded by the blood-brain barrier (BBB). It makes sense since we require a fully functioning brain to function. The BBB acts as a gatekeeper, controlling what substances are allowed to enter the brain and what remains excluded. Under normal circumstances, various toxins, pathogens, drugs and larger molecules are unable to cross this barrier.
The Blood-Brain Barrier
The blood-brain barrier (BBB) is a highly specialised and protective system that separates the bloodstream from the central nervous system (CNS). It serves as a selective barrier, controlling the passage of substances between the blood and the brain to maintain a stable and tightly regulated environment for optimal neural function. The BBB prevents harmful substances, toxins, and pathogens from entering the brain while allowing essential nutrients and molecules to be absorbed by neurones.
The BBB is formed through a combination of structural and functional components, including:
1. Endothelial Cells:
The inner lining of blood vessels in the brain is made up of specialised endothelial cells that are tightly joined together (in the same way gut lining cells are tightly packed together to form a barrier). These endothelial cells have specific characteristics that make them distinct from those found in other parts of the body. They are connected by tight junctions, which create a seal that restricts the passage of most substances (the same as the gut wall).
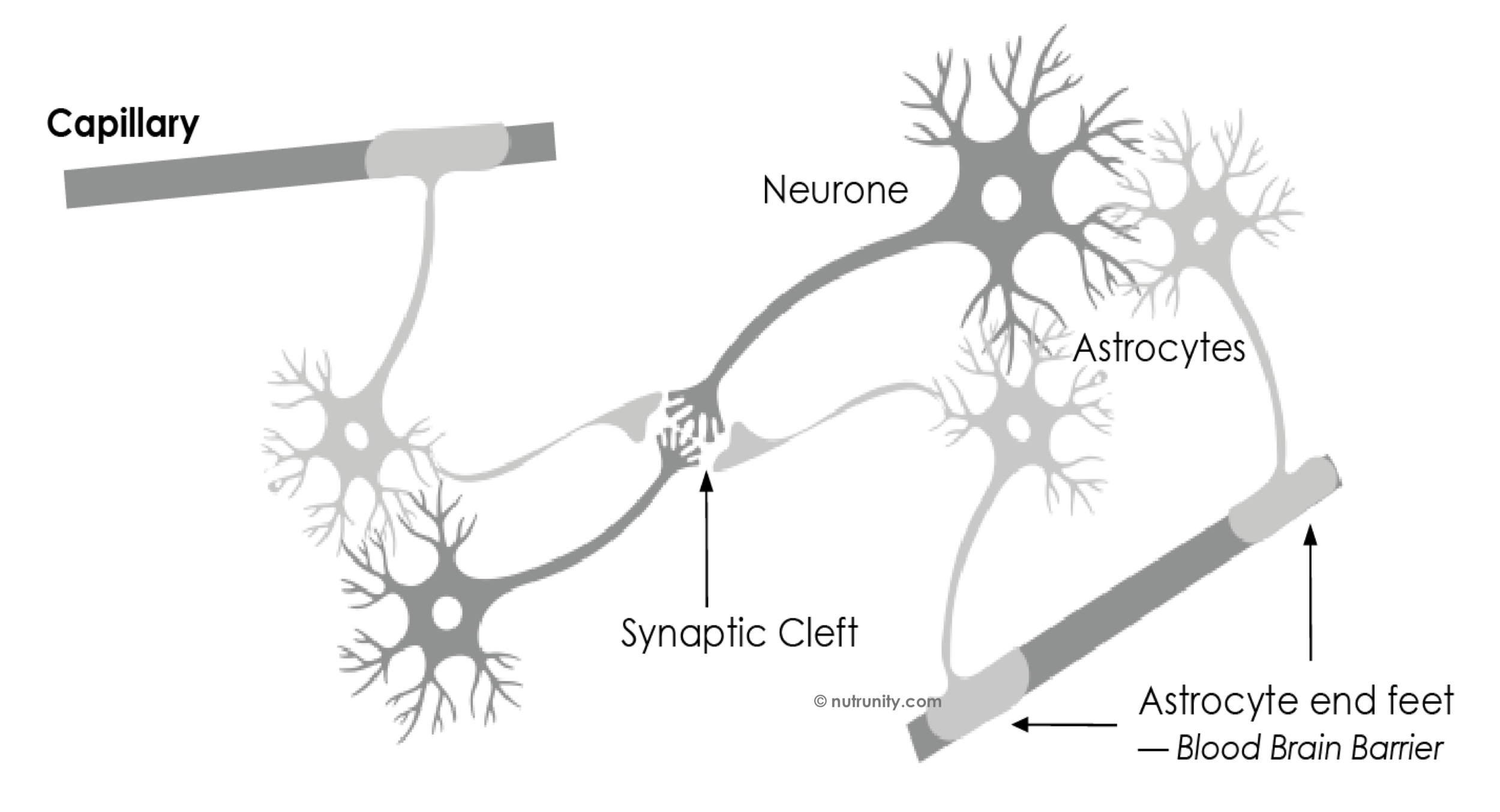
2. Astrocytes:
Astrocytes are star-shaped glial cells that surround blood vessels in the brain. They play a pivotal role in maintaining the integrity of the BBB. Astrocytes release chemical signals that help regulate the tightness of the endothelial cell junctions, influencing the permeability of the BBB.
Astrocytes and neurones connections, a bridge between the circulation and neurones.
Functions of the Blood-Brain Barrier
The BBB operates through several mechanisms:
Selective Permeability: The tight junctions between endothelial cells effectively limit the diffusion of large molecules, ions, microbes, and even some drugs from entering the brain. Gases, such as oxygen and carbon dioxide are able to pass through unrestricted. Some small, lipid-soluble molecules can pass through the BBB with relative ease.
Active Transport: The BBB employs transport proteins to regulate the passage of essential nutrients, such as glucose and amino acids, into the brain. These transporters ensure that vital substances reach the CNS in a controlled manner. Many different protein complexes are present on most body cell membranes. Each of them has a distinct role to fulfil, depending on where they are found if they are able to cross completely the membrane, virtually creating a bridge between the intracellular and extracellular spaces.
Efflux Pumps: These pumps help remove potentially harmful substances from the brain. One well-known example is P-glycoprotein, which helps protect the brain by pumping out drugs and toxins that may have crossed the BBB.
Metabolic Barrier: Enzymes within the endothelial cells can metabolise certain molecules before they can enter the brain, adding a layer of protection.
This level of protection can present challenges in drug delivery because it restricts the passage of many therapeutic agents. Researchers are continually working to develop strategies to overcome or bypass the BBB when necessary, such as for targeted drug delivery in the treatment of brain disorders.
We also know that the BBB can become permeable through the effect of radiation, and electrical currents (for example, placing a battery near the brain, or a mobile phone).
Neuroinflammation
Neuroinflammation, or inflammation within the brain, is a growing concern in neuroscience and medicine. When the brain's immune response is activated, it can disrupt the finely tuned balance of neural function, potentially leading to neurological disorders. This includes conditions like Alzheimer's disease, multiple sclerosis, and even mood disorders.
Recent animal studies have discovered a connection between gluten consumption and neuroinflammation. In what is believed to be a world-first discovery, researchers at New Zealand’s University of Otago have found wheat gluten causes brain inflammation.
Mice have very similar circulatory, reproductive, digestive, hormonal, and nervous systems to us, explains Professor Alex Tups, whose team published in the Journal of Neuroendocrinology.
The study investigated whether a low-fat diet or a high-fat diet, enriched with gluten, impacts metabolic markers or central inflammation, and is linked to weight gain. The focus was on the impact of gluten on the brain, particularly its role in inflammation processes. for the first time, the researchers found gluten-induced hypothalamic inflammation.
The hypothalamus is pivotal in regulating fundamental aspects of our physiology, including metabolism, blood sugar, and body weight. Additionally, it acts as an internal thermostat, continuously monitoring and adjusting various functions to maintain homeostasis. It also manages hunger, thirst, body temperature, and sleep, and it helps modulate energy expenditure.
Inflammation in the hypothalamus may disturb the intricate signalling pathways responsible for hunger and satiety, potentially leading to imbalances in food intake. This disruption can manifest as increased appetite, poor appetite control, and altered metabolic function, potentially leading to an increased risk of obesity and metabolic disorders.
“The brain has two types of immune cells similar to macrophages in the blood. These are called astrocytes and microglia. We found that gluten as well as high-fat diets (HFD) increase the number of those immune cells.
“The effect of gluten added to a normal diet increased the cell number to the same extent as if a mouse was fed a high-fat diet (HFD). When gluten was added to the HFD, the cell number went up even further.” Said Tups.
Why gluten is leading to hypothalamic inflammation is unknown.
Professor Tups adds: “Future studies need to reveal whether our findings in mice are translatable to humans.”
It is worth noting that the main sources of prebiotic fibre in the Western diet include grains and, particularly, wheat. This means that by cutting down on wheat, you are losing on health-supportive substances, and that you must find ways to optimise your intake of dietary fibre. There are other factors associated with regular gluten consumption. A study published in 2018 in Nature Communications discovered that a low-gluten diet affected certain bacterial species, such as Bifidobacteria.
The team reported that the abundance of 14 bacterial species of the 575 species identified was altered during the low-gluten diet and that “Consistently, the abundance of four species of Bifidobacterium was diminished during the low-gluten diet… This aligns with recent studies showing that healthy populations living traditional lifestyles have low or absent faecal abundance of Bifidobacteria compared with the intestinal ecosystems of individuals in industrial parts of the world. Thus the abundance of Bifidobacteria in adults living a Western lifestyle may to a larger extent reflect intake of diet enriched in wheat.”
Gluten-Free Products: A Double-Edged Sword
In response to the rising awareness of gluten-related issues, the availability of gluten-free products has increased exponentially. However, many of these products replace wheat and gluten-containing grains with alternatives like corn and rice. While they may seem like a healthier choice, these grains come with their own set of problems. Ultra-processed corn and rice can have a high glycaemic index, leading to rapid spikes in blood sugar, and severe dips in energy, and often crashes. These manufactured products also lack the essential nutrients found in whole grains, as well as fibre. Consequently, the excessive consumption of these grains may contribute to obesity and other health issues.
For example, rice cakes have a higher glycaemic index than pure sugar
An excessive intake of sugar and ultra-processed products also impact the gut and are found to contribute to leaky gut syndrome and gut inflammation, by directly impacting the production of short-chain fatty acids by commensal bacteria.
The Gut Microbiota
Gluten is found to increase intestinal permeability in everyone consuming it, in any quantity. The question is for how long and how often. Considering that every meal and snack in a Westernised diet contains gluten, some people may constantly bring damage to their gut without even knowing.
100% of people, including you, react to gluten in one way or another. You may not even notice it. Although, you may experience symptoms like bloating, discomfort or flatulence, or feel sleepy after a meal containing gluten. You may also find that your thoughts are muddled (brain fog), unable to think straight or control your mood or your emotions.
The Gut-Brain Axis
The gut-brain axis is a bidirectional communication system that connects the gut and the brain. It allows for constant interaction and information exchange between the two organs. A key player in this communication is the vagus nerve.
Dysregulation of the gut-brain axis can lead to disturbances in mood, cognition, and even neuroinflammation. Gut inflammation can participate in the release of histamine, endotoxins, alcohol and other pro-inflammatory metabolites that can irritate and inflame the liver. An inflamed liver can also be a device factor in neuroinflammation.
The vagus nerve, flow of information and main functions.
To the question, is going gluten-free a better option than eating gluten daily?
As usual, the answer is “it depends!”
If you are going gluten-free but continue to consume ultra-processed and junk foods, then you probably think you are choosing the lesser evil. Gluten-free and so-called healthy foods, if processed to the point there is nothing close to what nature intended then it is probably unhealthy.
If it contains excessive amounts of sugar, then it is best to steer away from those completely. By now, you should know that excessive intakes of sugar are linked to overexpressed inflammation processes and pain.