Men Fertility
UK HEALTH RADIO INTERVIEW (Transcript)
Is there a physiological factor that may affect male fertility?
Indeed, there is. As a male child grows, it is often routine for doctors to check that the testes have descended. In other words, they check that the testes have moved to their normal place in the scrotum.
We know that men with undescended testes tend to have a higher infertility rate compared to the general population, especially those with a history of bilateral undescended testes. The rate is also higher compared to those with unilateral cryptorchidism. A fancy term for undescended testes. We can note here that it can be one or both testes that have yet to migrate to the scrotum.
Cryptorchidism is the most common birth defect involving the male genitalia. The rate is about 3% for full-term male infants. It increases dramatically to 30% in preterm babies.
In 80% of cases, the testes descend by the third month. But, the testes can be as high as the upper part of the lower abdomen, like near the waistline. They can also be located anywhere around the groin area and the legs.
It is also important to note that for men with undescended testes, the risk of developing testicular cancer increases 4 to 7 times compared to the general population. This is not something to take lightly.
For information, the testes develop in the abdomen in a growing foetus. By the way, as a tissue, they are closely related to the kidneys. As development progresses, the testes naturally migrate to the groin area and finally into the scrotum.
When I am dealing with infertility in clinics, this is a question I ask, because, from experience, half of the cases in difficulties conceiving implicate the male partner.
There is a multitude of factors and our role as health practitioners is to identify the causes that make conceiving difficult.
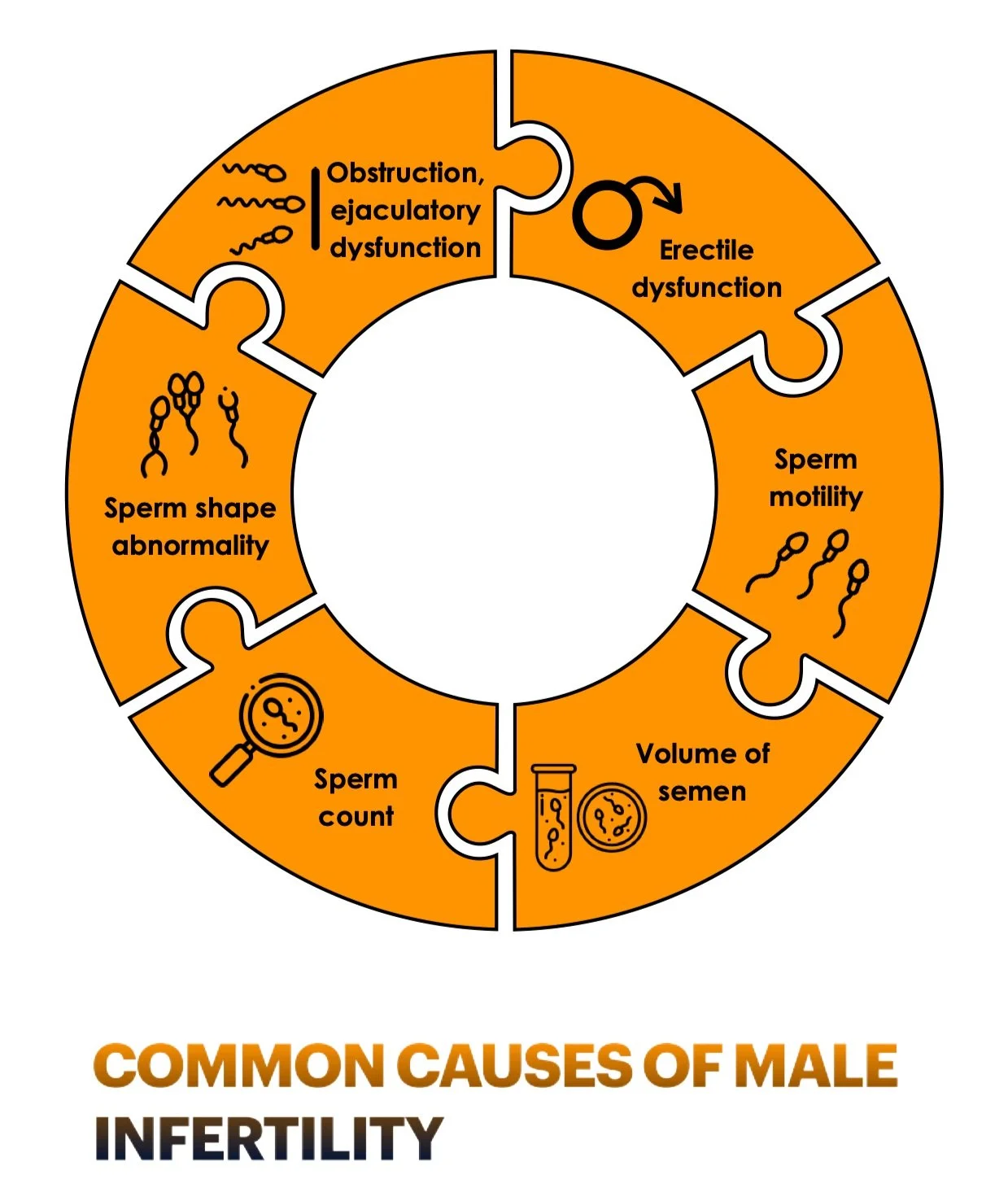
Infertility affects up to 15 per cent of couples. And we know that the quantity and the quality of sperm are also extremely important. Azoospermia or the absence of motile and, therefore, viable sperm in the semen is found in nearly 20 per cent of the infertile male population. So, it is important to determine the factors affecting male fertility.
Male infertility can be classified into three major groups:
Non-obstructive infertility
Obstructive infertility and
Coital infertility
Let’s look at these in more detail:
Non-obstructive infertility. It accounts for 60% of cases. It includes anything that leads to inadequate sperm production by the testes. It could have a genetic factor or occur as a result of hormonal imbalances.
This is where undescended testes, as we have just discussed, fall into.
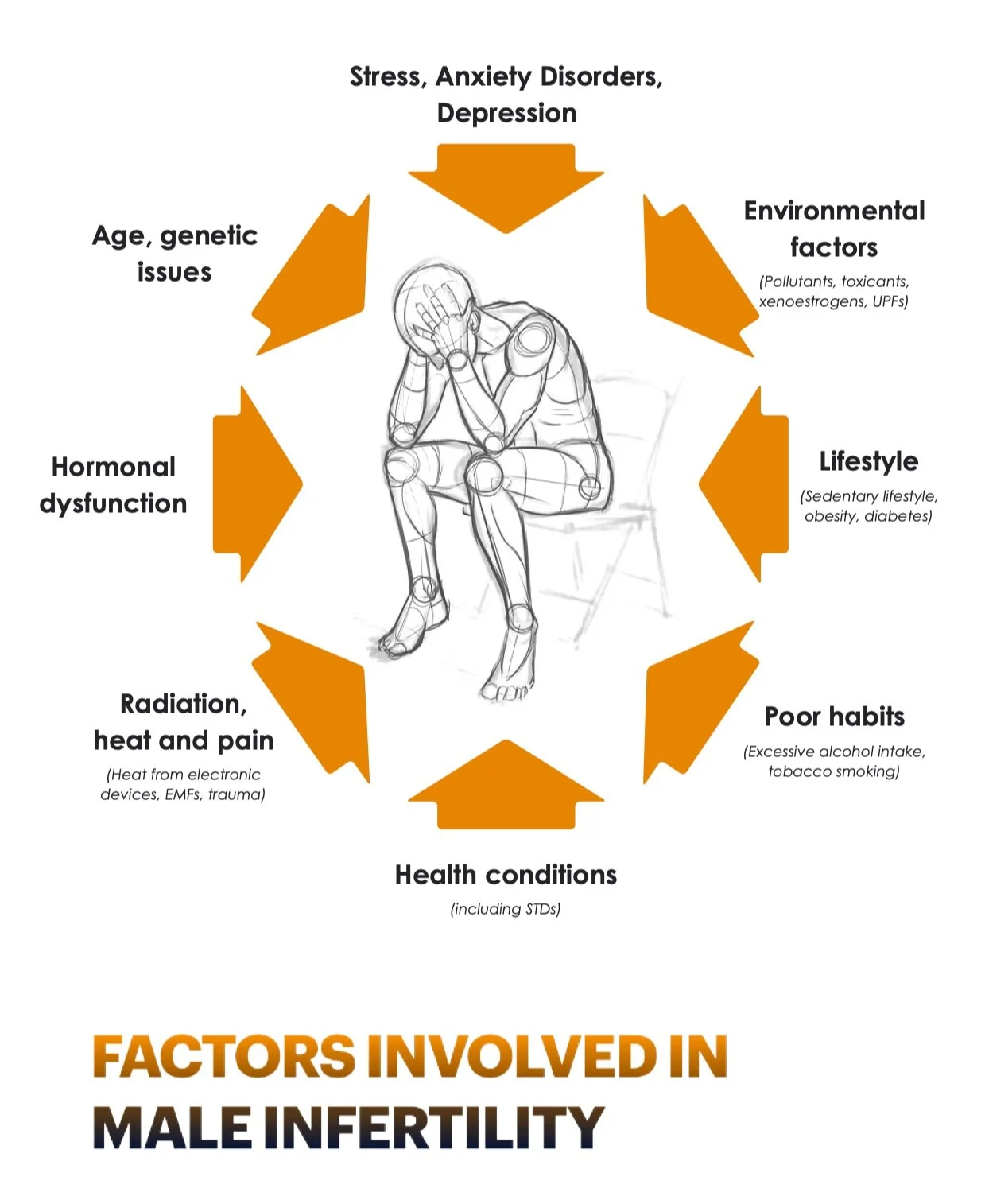
Some toxins may also be involved. Those are known as gonadotoxins. We immediately think about heavy metals, and indeed they belong to this category, but we can also add certain medications and recreational drugs, tobacco smoking and excessive alcohol intake, as well as organic solvents and pesticides. As we would expect, radiation and chemotherapy can also contribute to the problem.
Obstructive infertility. As the name indicates, there is a blockage in the genital tract. There is normal sperm production, but it is not able to exit the testes.
In about 2% of cases, coital infertility is secondary to sexual dysfunction, which impairs the ejaculation process or intromission (that is sexual intercourse. Erectile dysfunction is a major component as it is involved in at least 33% of all cases of male infertility). Old age is also a contributing factor that falls into this category. But, I also want to add anything that affects mental health, so chronic stress or anxiety disorders, for example, even depression, but it can also be having a lot on your mind or being mentally and physically exhausted.
Here, I also include burnout and similar problems. It is very difficult to mentally think about performing when there is already so much preoccupying the brain and weighing on your shoulders.
Also, we know that stress and the dominant role of cortisol, the stress hormone, can affect hormone levels as well as neurotransmitters and also impact detoxification processes, which means that cells may have more difficulties detoxifying no longer needed neurotransmitters, principally dopamine and epinephrine (adrenaline). Chronic stress can also affect liver function and the elimination of detoxified hormones, which may be further exacerbated by chronic constipation and, therefore, a toxic colon. Your colon can become toxic due to the retention of waste and allow for the reuptake of detoxified hormones which will once again travel in the bloodstream and exert some activity until they are once again detoxified by the liver.
Gonadotoxins — medications:
Allopurinol, Colchicine, Cimetidine, Corticosteroids, Cyclosporine, Diltiazem, Erythromycin, Gentamicin, Methotrexate, Neomycin, Nifedipine, Nitrofurantoin, Opioids, Tetracycline, Spironolactone, Sulfasalazine, and Ketoconazole. Chemotherapy (e.g., Cisplatin and Carboplatin, platinum-based agents used to treat testicular cancer) and other anticancer drugs like topoisomerase inhibitors (inhibit cell proliferation by preventing DNA replication, stimulating DNA damage, and inducing cell cycle arrest)2 or alkylating agents (highly reactive compounds that attach to DNA and cellular proteins. May induce azoospermia within 90 days. i.e., Cyclophosphamide, Busulfan, Chlorambucil, Procarbazine, and others).
Suspected medications:
Ibuprofen (may decrease sex hormones; however, it has not been shown to cause infertility, lower testosterone levels, or decreased sperm count.[1]
Other drugs and toxins:
Nicotine (e.g., tobacco smoking or patches, including passive smoke exposure), excessive alcohol intake, anabolic steroids, anti-androgens, cocaine, marijuana, and opioids.
Heavy metals, organic solvents, and pesticides.[3]
What are the suspected factors involved in male infertility?
With a male factor being a primary or contributing cause in approximately 50% of couples failing to conceive, then it makes sense to uncover the contributing factors.
The causes of male subfertility can be various. There can be congenital, acquired or idiopathic components that impair spermatogenesis or the quality of sperm, as well as the motility of sperm. Many health conditions can affect male fertility, this is why we have an important role to play in identifying contributing factors.
Although semen analysis remains the cornerstone for evaluating male infertility, I also rely on advanced diagnostic tests to investigate sperm quality and function.
As a naturopathic practitioner, I also want to uncover imbalances and identify factors that may be contributing to the problem. I always look at the individual as a whole, not as a problem to treat. Therefore, I want to know everything about diet, lifestyle, sleep, and stress, or anything that may affect the normal functioning of the body.
I also aim to identify and rectify malnutrition, or nutrient deficiencies. We know that, for example, vitamins C, D, and E, and CoQ10, are important
for sperm health. Selenium is also needed for normal sperm production and development. Spermatozoa are made up of a higher concentration of omega-3 fatty acids.
Other nutrients like Vitamin B12 and folate are needed for DNA synthesis and protection and sperm quality. Any deficiency may be implicated in poor transcription and replication. According to studies, low folate levels in semen were associated with poor sperm DNA stability. Folate is, therefore, a nutrient not only necessary for female fertility but also for male fertility. When I accompany a couple trying to conceive, I usually suggest a multivitamin complex with sufficient levels of B vitamins, even if the diet appears to be impeccable.
Additionally, I want to know the cause of hormonal imbalances or insufficiencies or anything that can affect the hypothalamic-pituitary-gonadal (HPG) axis. It is also important to note that the parasympathetic nervous system controls erectile function while the sympathetic nervous system is responsible for emission and ejaculation.[4] This means that a man needs to be relaxed first, then stressed to ejaculate.
This is, therefore, no simple task.
Since a higher concentration of stress hormones negatively impacts sex hormone levels and the quality of sperm and also reduces spermatozoa functionality, chronic stress cannot be ignored when it comes to male or even female infertility.
According to research, psychological stress can decrease testosterone levels and thereby affects seminal quality by decreasing sperm count motility and spermatozoa morphology.5
Since stress hormones are also involved in inflammation processes, oxidative stress could be another cause of male infertility. Indeed, it has been found to adversely impact semen and sperm quality and fertility. Stress can be psychological as just explained, but infections and inflammation are also huge stressors for the body as they require a huge amount of energy for the body to deal with the problem. The body thus doesn’t have any energy to spare and reproduction is not an essential task during this time.
Inflammation also leads to oedema and intratesticular pressure as observed in ascending urogenital tract infections such as post-gonorrhoeal and chlamydial infections. Typically this can occur after the blood-testis barrier has been compromised, as in the case of trauma, testicular surgery, varicocele, and orchitis. A varicocele is an enlargement of the veins within the loose bag of the scrotum, thus impacting the temperature). Orchitis is a term used for pain and swelling of one or both testicles.
In very extreme circumstances, the body can also produce anti-sperm antibodies, a form of autoimmune infertility, which means that spermatozoa are attacked by the immune system as a result of damage to the blood-testis barrier.
Another issue that is rarely discussed includes radiation and electronic devices. The scrotum is always 2 degrees lower than the rest of the body. It appears to benefit the production of sperm and the quality of sperm.
Resting a laptop on your knees or keeping your mobile phone in your trouser pockets can raise the temperature. Furthermore, studies show exposure to heat and electromagnetic fields (EMFs) given off by computers and mobile phones can affect male reproductive organs and sperm quality. Although sound research is still lacking and we are still trying to catch up to new technologies and understand their effect on human biology. It may be some years before we understand the extent of the problem. We are virtually the guinea pigs of our modern times.
Since studies have found that men keeping their knees together for prolonged periods can generate enough heat to decrease sperm viability,[6] adding more heat by the regular and long-term placement of a laptop o your lap is bound to cause a rise in temperature, which is spermatotoxic and can kill sperm. Interestingly, scrotal shielding with a lap pad does not protect from scrotal temperature elevation due to the prolonged periods of keeping the legs together.
This may be a reason why most men unconsciously sit their legs wide apart as if slouching was the natural way for man to keep their genitals cooler.
What do you think is one main factor involved in male infertility?
A meta-analysis suggests that the increased frequency of male reproductive abnormalities reflects adverse effects of environmental or lifestyle factors, such as occupational and environmental exposures, medications, and sexually transmitted diseases.
These factors play a key role in determining reproductive health and can influence fertility.
Over the last few decades, there have been progressive changes in aspects of our diet, lifestyle as well as environment. A tsunami of reports has exposed the incidence of male infertility in recent years, which tends to increase as a result of various factors such as environmental pollution, stress, and lifestyle.
As discussed earlier, factors such as tobacco smoking and excessive alcohol intake, but also high temperature, and some electronic devices, all seem to have a profound negative impact on general health and the deterioration of reproductive health. All these factors may impair male fertility by interfering with spermatogenesis (the production of sperm), spermiogenesis (the final stage in the production of spermatozoa), sperm motility, sperm DNA and chromatin integrity (the formation of chromosomes, the genetic make-up that is passed on to build a brand new human being from scratch), hormonal regulation or by reducing the fertilising capacity of spermatozoa.[7,8]
Clinical evidence also tends to shed a light on the way men live their lives. What we see are ultra-stressed men who seem to have so much on their shoulders that there is never time to relax and enjoy some quiet time and much-needed intimacy with partners. It’s all work work, and taking work back home, burning the midnight oil and the candle at both ends.
Burnout or the early stages of adrenal fatigue already set the individual on a path toward dysfunction, and eventually, ill health and difficulties conceiving. It is a very important factor to take into consideration as a person trying to conceive but also for us practitioners.
The issue here as well is that we are all living life at full speed and there is rarely enough time to pack all the things that need to be done in the day most couples are feeling the constant pressure of life and, therefore, stress may be the major problem affecting both partners. Failing to conceive may also add even more pressure and anxiety and the conventional route can often lead to heartbreaks. Couples need to support each other during these difficult times because of the traumatic experience of it all.
So if we add up all that play against our biology, and our endocrine system and disturbs the fragile equilibrium between our hormones, we are now faced with even more challenges as a result of living in a constantly connected world.
A report brought forward to the European Commission over a decade ago exposed a very problematic aspect of male reproduction and there has been recent controversy regarding changes in sperm counts during the past 60 years worldwide. It has been reported widely in the last two decades that sperm count is declining — a reported 32% decline in sperm count from 1989 to 2005 has been reported.9 The deterioration of semen qualities was already reported in the 1970s. Even if studies show some inconsistencies and the parameters used, the trend cannot be ignored. There are meta-analyses covering over 60 papers that included 15 000 men from 23 countries all showing a net reduction in sperm count and quality of sperm.
What the studies looked at were factors including environmental and occupational exposure, and those included pesticides, heavy metals, and other endocrine disrupters. They also looked at lifestyle factors like usage of cell phones, laptops, wi-fi, and consumption of alcohol and tobacco. Using those two factors they looked at the direct effect on human cells, including oxidative stress (or the creation of free radicals), cell damage, and possibly cell death, and they also looked at the impact of those factors on the hypothalamus-pituitary axis that could lead to low concentrations of testosterone.
Since testosterone is required for spermatogenesis any factor with endocrine-disruptive capabilities will affect reproduction. Insulin dysfunction is also involved as it can dysregulate many pathways and also the way the body handles blood sugar and blood lipids, and, therefore, inflammation. Inject a little cortisol here and there, every day, and even the insulin system will be struggling to maintain balance. The pressure placed on the thyroid and the impact on the conversion of thyroid hormones from T4 to T3 may also be heavily impacted, affecting every tissue in the body.
Now if we look at the last factor from the meta-analyses, which included primary pathologies of the male reproductive system but also systemic pathologies like diabetes, thyroid disorders, adrenal hyperactivity, and, of course, obesity. As the paper noted, since pathologies seem to be more prominent with age, an ageing man may find conceiving more and more difficult, as all of those factors can lead to low sperm count.
Being overweight or obese was associated with an increased risk of oligozoospermia (low sperm count) or azoospermia (poor sperm motility). Obesity can really derail the body but it also affects the concentrations of hormones and their mode of action, including disrupting sperm DNA integrity the genetic makeup that is used to make a new human being from scratch.
Obesity is such a major contributor to man fertility that a paper published a few weeks ago placed an emphasis on the concept of obesity-mediated male infertility, which, according to the researchers, needs timely updates and a pristine understanding.[11]
The WHO reported worldwide obesity had more than doubled since 1980. They also reported, in 2014, that more than 1.9 billion adults 18 years and older were overweight. Of these, over 600 million were obese. Over one-third of male adults aged 18 years and over were overweight in 2014. Since men tend to accumulate weight as they grow older, the prevalence of obesity increases with age, placing more pressure on the reproductive system and can play a decisive role in fertility. problems.
So, let’s go back to endocrine disrupters and other compounds that can affect male reproduction. Reports and animal studies have exposed that some pesticides have been known to affect testicular functions, caused testicular atrophy,[10] or rendered thousands of agricultural workers sterile in many countries worldwide due to occupational exposure.[12]
There are dozens of peer-reviewed studies that show the negative impact of environmental toxicants.[8]
There are also thousands of chemicals that have not yet been included but yet there is experimental evidence of testicular toxicity in animals for which data are not available for humans. Among thousands of chemicals that we are exposed to environmentally or occupationally, including pesticides, very few have been evaluated for reproductive toxicity, specifically in various age groups of men. This is a problem because the susceptibility to be exposed to these chemicals increases with age.
Plastics are also a huge problem, including BPA and phthalates, simply because we are exposed to these compounds daily and to a lot of them. They can be found in cosmetics and personal care products, perfumes that are used on the skin or indoors, and also in detergents and fabric conditioners. Phthalates, for example, can make up to 20% of the final product and yet be labeled under the word “perfume”.
The key issue here is that many endocrine disrupters are bio-accumulable, which means they may be retained within the body and accumulate with continuous exposure and reach dramatic levels as a man ages. This is why age is one of the key factors in failing to conceive. Again, if cumulate all that is playing against our bodies, the combination of toxicants, chronic stress and anxiety, bad dietary choices and poor lifestyle habits, and chronic lack of sleep, we can now understand why our hormones are out of balance and the tremendous pressure on our endocrine system.
But by far the most prominent factors that are of increasing interest are ionising radiation and heat.
As the use of cell phones, laptops, and Wi-Fi has increased tremendously in the past three decades, the possibility of a radiation-induced decline in sperm count may follow the same trend. Since the majority of people do not switch off their routers at night or even their mobile phones, the human body is exposed to radiation every second of every day and every night.
This is not innocent and we are paying the price according to a tsunami of medical papers. In my upcoming book Detox before Energise, I am exposing the main toxicants and endocrine disruptive agents that we are exposed to daily, including EMFs, and their impact on our biology. If they can affect our health it is only natural that they may lead to fertility issues.
More in Part 2 of the interview, scheduled for late 2022-early 2023.
References:
Kristensen, DM. et al. (2018). Ibuprofen alters human testicular physiology to produce a state of compensated hypogonadism. Proceedings of the National Academy of Sciences of the United States of America. 115(4), E715-E724. doi:10.1073/ pnas.1715035115
Liu, J. et al. (2019). Topoisomerase inhibitors promote cancer cell motility via ROS-mediated activation of JAK2-STAT1-CXCL1 pathway. Journal of Experimental & Clinical Cancer Research. 38, 370. doi:10.1186/s13046-019-1353-2
Moses, S. (2022). Gonadotoxin. Aka: Gonadotoxin, Medications that Impair Male Fertility. Available at: https://fpnotebook.com/uro/ Pharm/Gndtxn.htm. Last accessed: Oct. 7th, 2022.
Friedman, SK. Dull, RB. (2012). Male infertility: An overview of the causes and treatments. U.S. Pharmacist. 37(6), pp. 39-42.
Bhongade, MB. et al. (2014). Effect of psychological stress on fertility hormones and seminal quality in male partners of infertile
couples. First International Journal of Andrology (Andrologia). 47(3), pp. 336-342.
Sheynkin, Y. et al. (2011). Protection from scrotal hyperthermia in laptop computer users. Fertility and Sterility. 95(2), pp. 647-651.
Sengupta, P. et al. (2018). Decline in sperm count in European men during the past 50 years. Human & Experimental Toxicology. 37(3), pp. 247-255.
Sengupta, P. Dutta, S. Krajewska-Kulak, E. (2017). The disappearing sperms: Analysis of Reports Published Between 1980 and 2015. American Journal of Men's Health. 11(4), pp. 1279-1304. doi:10.1177/1557988316643383
Rolland. M. et al. (2013). Decline in semen concentration and morphology in a sample of 26,609 men close to general population between 1989 and 2005 in France. Human Reproduction. 28(2), pp. 462-470. doi:10.1093/humrep/des415
Torkelson, T. (1961). Toxicological investigations of 1,2-dibromo-3-chloropropane. Toxicology and Applied Pharmacology, 3, 545Torkelson T. (1961). Toxicological investigations of 1,2-dibromo-3-chloropropane. Toxicology and Applied Pharmacology. 3, 545
Chaudhuri, GR. et al. (2022). Obesity and male infertility: multifaceted reproductive disruption. Middle East Fertility Society Journal. 27, 8. doi:10.1186/s43043-022-00099-2
Whorton, D. et al. (1977). Infertility in male pesticide workers. Lancet. 2, pp. 1259-1260